The discovery of antibiotics was a revolution in medical practice, and their use in surgery has led to considerable advances that have benefited millions of patients. In the 1980s, the risk of postoperative infection, one of the major complications of surgical procedures, led to a better definition of the role of antibiotic prophylaxis in surgery. Two consensus conferences, organized by SFAR (Société française d’anes- thésie et de réanimation) in 1992 and 1999, put forward practical recommendations for antibiotic prophylaxis in orthopedic and plastic surgery. These recommendations, which have a strong medicolegal value, are not all scientifically validated, however, and many are based on extrapolation from data validated for prosthetic hip surgery or the management of open leg fractures, in the absence of available data.
However, hand surgery, the natural offspring of orthopaedics and plastic surgery, is not singled out in these consensus conferences. Postoperative septic complications are much less frequent in hand surgery, and the SFAR proposals may not be adapted to the day-to-day practice of hand surgeons. In addition, the worrying increase in bacterial resistance, widely reported in the media and echoed by the public, has led doctors to redefine the optimal use of antibiotics in terms of benefit/risk for the individual and society. The Société française de chirurgie de la main (French Society of Hand Surgery), keen to help hand surgeons in their professional practice, felt it necessary to propose a scientifically reasoned attitude to the practice of antibiotic prophylaxis in hand surgery, and it is this work, carried out in 2003 and presented at the annual congress in December 2003, that is the subject of this publication.
1. Introduction
J.P. Lemerle: Consultant, Department of Orthopaedic Surgery (Pr Doursounian), Hôpital Saint-Antoine, 184, rue du Faubourg-Saint-Antoine, 75571 Paris cedex 12, France.
Raymond Vilain’s deliberately restrictive attitude to antibiotics in the 1970s naturally led surgeons to give priority to pre- and intraoperative hygiene, and to making their procedures as atraumatic as possible. The validity of these “intuitions” is clear today, when the relationship between antibiotic infla- tion and germ resistance is obvious. But over time, medico-legal fears, routine and unsubstantiated personal opinions have led to a tendency towards systematic antibiotic prophylaxis. There are some consensus-based proposals for codifying antibiotic prophylaxis in orthopaedics. However, these are very general and do not cover the very specific field of hand surgery, except by analogies whose scientific validity has not been established. The aim of this work is precisely to propose an attitude
in documented situations, leaving everyone free to make their own choices in those that are not yet documented.
“This work will have to be continued as publications on the subject appear. This work will have to be continued as publications on the subject are issued, but it already constitutes a binding reference.
2. Current prevalence of postoperative infections
J.R. Werther: surgeon, orthopedic surgery department (Pr Doursounian), Hôpital Saint-Antoine, 184, rue du Faubourg-Saint-Antoine, 75571 Paris cedex 12 and Clinique Rémusat, 21, rue de Rémusat,75016 Paris, France.
It’s often said that the best studies should be prospective, randomized and double-blind. But they must also be clinically relevant, i.e. the statistically demonstrated benefit must be of interest: it’s not enough to be “statistically significant”, the expected benefit must also be evaluated, preferably a priori. In particular, it’s a question of seeing how many patients need to be treated to avoid an adverse event, which must also be “significant”.
We conventionally choose an “alpha” risk (risk of wrongly concluding a difference) of less than 5%. For the conclusions of a study to be valid, it must also be sufficiently “powerful”; i.e., the risk of not seeing a difference that exists must, by convention, be less than 20%.
The first phase in designing a study on anti-bioprophylaxis assumes that the rate of infection without anti-biotics is known. This rate is generally found in the literature.
For hand surgery, the rates found in the literature are extremely varied (from 0.3% to 15%), which makes it impossible to choose a reference rate. which should be included in the control group of all studies, otherwise there would be a considerable loss of power.
We therefore decided to determine an infection rate for hand surgery. The criteria proposed in the literature for defining surgical site infection (SSI) are surprisingly variable. We have decided to adopt very restrictive and binary criteria. Only patients with :
- initially operated on by a qualified hand surgeon, which in our view guarantees mastery of trimming and atraumatic surgery. We did not consider it advisable to include patients who had been sutured in the emergency department, or closed in tension without trimming… ;
- excluding primary infection (panaris, phlegmons or morsu-res);
- excluding infection following necrosis
We excluded patients who did not require revision surgery.
To get an idea of this infection rate, we carried out a retrospective multicenter study using the major hand surgery centers with which we had close relations.
Six centers were contacted, and three responded (Boucicaut/HEGP/Saint-Antoine: Dr Werther; Urgences Mains Val-de-Seine: Dr Barbato, and SOS Mains Nantes: Dr Chaise): Dr Chaise), these three centers do not practice any antibiotic prophylaxis. Twenty-two thousand (22,000) patients were included in this study, and there were a total of 21 reworkings for infec- tions, a rate of 1 ‰.
Based on these data, we can pre-calculate the number of patients needed to demonstrate a benefit from antibiotic prophylaxis. A study looking for a 50% reduction in the rate of infection, with 80% power, would require the inclusion of 91,000 patients.
1.1 Comments
The rate found in this study is lower than that generally reported in the literature. It is most likely underestimated Some repeat surgeries may have been “forgotten”, some patients may have moved to another center, and surgeons are often less inclined to repeat their own patients if infection is suspected.
That said, in favor of the value of this work, it should be noted:
- that the observed rate is remarkably constant on all three sites;
- that in published studies, the rate of rework due to infection, when reported, is less than 1%, i.e. fairly close to the observed rate.
One well-documented study found a surgical site infection (SSI) rate of around 15%. This very high figure is not found in any other study of surgical site infections in the literature. There are several possible conclusions to be drawn from this study:
- if we assume that it’s accurate, the calculations that
show that we no longer need 91,000 patients in a prospective study aimed at halving the rate of SSI, but 850. This more “reasonable” figure, however, already corresponds to a large-scale study with a high cost, and such a study has never been carried out to date;
- the question arises as to the extent to which statisticians
consulted in the above-mentioned study did not, in good faith, modify the judgment criteria in such a way as to obtain sufficient power. In order to carry out a study with a chance of obtaining significant results, even with an infection rate at this level, a very broad definition of infection is required, which means that patients who recover without sequelae with local care (i.e., in practice, who recover on their own) are included as infected, in a proportion of 50:1. However, there is no evidence to suggest that lowering the rate of benign infections will lower the rate of serious infections.
1.2 A new prospective survey?
Statistical studies compare events. Il faut qu’un certain nombre d’événements se produisent dans cha-
group (around 50 for a 50% reduction) to judge statistical significance. These studies are different from more “classic” studies that compare averages (of pain, mobility, strength or a usual arbitrary score), where each patient contributes to the power of the study.
In the case of antibiotic prophylaxis, patients who do not become infected make no contribution to the study, and represent at least 99% of the population to be included. The number of patients treated “for nothing” must be weighed against the risks of antibiotic therapy for both the patient and the community. A study on antibiotic prophylaxis, with a surgical revision rate of 1 ‰ would be of no clinical interestIt is not reasonable to treat 2,000 patients to avoid a recurrence. By way of comparison, in large car-diovascular studies, the limit is considered to be treating 100 patients to avoid a major stroke…
In practice, prospective randomized studies are never carried out for events with a frequency of less than 15%. In practice, therefore, a prospective, randomized study of antibiotic prophylaxis in hand surgery is not only technically unfeasible, but would not yield any significant results, given the low rate of repeat surgery in our specialty.
References: Bouyer et al. Epidemiology: principles and quantitative methods, pp. 440-450; Éditions Inserm, Paris 1995.
3. Survey on the current practice of antibiotic prophylaxis by members of the French Society of Hand Surgery
- Tchenio: Assistant clinical supervisor, orthopedic surgery department (Pr Doursounian), Hôpital Saint-Antoine, 184, rue du Faubourg-Saint-Antoine, 75571 Paris cedex 12, France.
- Vercoutere: assistant clinical supervisor, orthopedic surgery department (Pr Augereau), Georges-Pompidou European Hospital, 43, rue Leblanc, 75015 Paris, France.
The work was carried out in preparation for the round-table discussion on antibiotics at the GEM 2003 winter congress. We have excluded from this work clearly codified situations such as human or animal bites, where the systematic prescription of antibiotics is little discussed.
- The questionnaire
This is a questionnaire sent to each of the 291 members of the society. It summarizes the most frequently encountered clinical situations, both in emergency and closed surgery. It is presented in the form of a decision tree.
The proposed answers are deliberately yes or no, in order to obtain clear answers for a strong consen- sus. It was important to us that the questionnaire could be completed quickly; several attempts with the department’s surgeons enabled us to verify that the average response time was around three minutes.

To avoid visit reminders telephone useless, we have requested à each from specify sound name, and we we are interested at type exercise, à the research from differences from requirements between activity liberal or publi– that.
3.2 Collection of data

Data was collected both by regular mail and via the GEM website (http://www.gem-sfcm.org), where the questionnaire was placed online to increase the number of possible responses. We received 168 responses, 144 by post and 24 electronically. Although the response rate by post was higher than that by electronic means, we were still able to obtain the best possible response,
we believe that the Internet is an interesting means of communication because of the ease and speed with which the data obtained can be used. If this mode of communication becomes the norm, we should be able to achieve higher response rates in the future.
3.2 Results
3.3.1 Comparison public–private
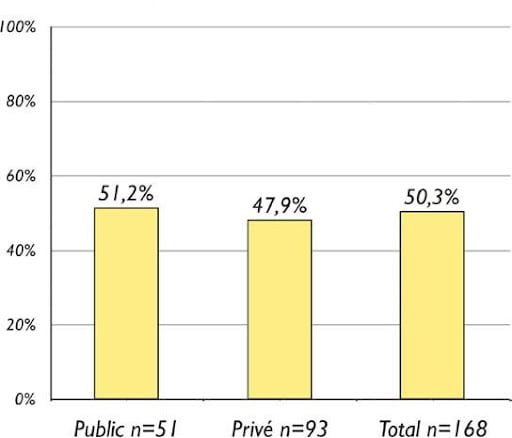
We visit a rate from prescription antibiotics superior in visit hospitals, but this difference is not statistically significant.
3.3.2 Questionnaire Emergencies
3.3.2.1 Parts soft.

Visit case reach exclusive from parts soft, visit criteria which influential positively the prescription are the character soiled initial, damage a organ noble, and the classic deadline from plug at load superior or no à six hours.
3.3.2.2 Fractures closed.

In case of fracture closed, more than third of surgeons
3.4 Controlled soft-tissue surgery


For the majority from gestures at surgery set, absten– tion prevails ; visit criteria influencing mainly on visit requirements are inclusion from equipment (prostheses, im- plants…) and the surgery from recovery.
3.5 Summary of factors that influence on the prescription antibiotic at within of the SFCM
3.6 prescribe a antibiotic therapy ; the rate of prescription is
little influenced by the type of osteosynthesis.
3.3.2.3. Fractures fractures.
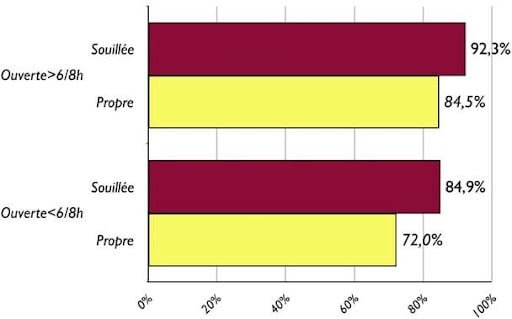
Visit fracture open remains for the majority from colleagues, a indication formal antibiotic therapy, what that or the deadline from plug at charge.
Emergencies Controlled surgery Soiling Bone and/or joint procedure Response time > 6-8 hours Revision surgery
Damage to noble elements Implant placement Bone and/or joint damage
Skin opening for bone or joint injuries
Hardware inclusions
4. Methodology
C. Dumontier: hospital surgeon, associate professor at the Collège de Médecine des Hôpitaux de Paris, orthopedic surgery department (Pr Doursounian), Hôpital Saint- Antoine, 184, rue du Faubourg-Saint-Antoine, 75571 Paris cedex 12 (christian.dumontier@sat.ap-hop-paris.fr) and Institut de la Main, 6, square Jouvenet, 75016 Paris (ch.dumontier@gsante.fr).
The aim of this conference was to provide practitioners with recommendations for good practice based on the following
data reliable and validated. The ideal would have summer from go to a conference from consensus as the proposes ANAES. Mal- fortunately, the conference, such it is proposed by ANAES, assumed a investment minimum from 150 000 Q, incompatible with our budget and a deadline from production of approximately two years then that we do arrangements that a year. After several contact with visit responsibility bles from ANAES, from AFSSAPS, at infectiologists and after reflexion, we have agreed :
- that it was not possible for us to scrupulously follow the criteria for a consensus conference as proposed by ANAES;
- that we would not have sufficient funding;
- that these criteria are adapted to broad issues (antibiotic prophylaxis in surgery, for example, as defined by the SFAR), whereas the problem posed by hand surgery was, on the contrary, very limited;
- but that we could, within the company and through our
professional relations, build up the equivalent of such a conference at a lower cost, which, even if it didn’t have the imprimatur of ANAES, would nevertheless have sufficient scientific (and therefore medico-legal, as it fills a referential void) value for hand surgeons to be able to use it if they so wished.
We have therefore built this conference as closely as possible on the recommendations of ANAES (ref.: Les confé- rences de consensus, base méthodologique pour leur réalisa- tion en France (Conférences de consensus – 1997 – réactua- lisation 1999), available for download at www.anaes.fr ).
First, in November 2002, we set up an organizing committee to define the subject, select the members of the various committees and the jury, and ask the questions of the jury.
4.1 Committee Committee
Professor Lemerle, hand surgeon, consultant, expert to the French Supreme Court, President of the French Society of Hand Surgery.
Professor Vildé, Head of Infectious Diseases Department, Hôpital Bichat, Paris.
Professor Gilles Chatellier, epidemiologist and public health, Georges-Pompidou European Hospital, Paris.
Doctor Christian Dumontier, surgeon.
4.2 A committee of reading committee
It was set up in November 2002.
It is responsible for researching all the data available in the literature and retaining only relevant articles, using the reading criteria defined by ANAES (Guide analyse de la littérature et gradation des recommandations). using the reading criteria defined by ANAES (Guide d’analyse de la littérature et gradation des recommandations).
- January 2000 – available for download at www.a- naes.fr). These criteria, together with a copy of a Cochrane search on an equivalent subject, were given to the reading committee to help them in their search (for the record, Cochrane groups are literature analysis groups which, on a given subject, search for relevant references, analyze them and, if possible, give recommendations for good practice. To access the site, go to www.cochrane.org and references for the “muscu- losketal group” can be found at http://www.cochrane.org/ cochrane/revabstr/MUSKINJAbstractIndex.htm ).
This committee was initially made up of five surgeons and an anesthetist, but given the lack of involvement of most of these members, a second, smaller committee was formed, comprising Drs. Tchenio and Dumon- tier, assisted by Dr. Vercoutere, all hand surgeons.
This reading committee provided the group of experts with a summary of the literature (and copies of all the articles, which were not very numerous, were included in the bibliography). To facilitate their work, each expert was in charge of a single chapter (e.g. bone surgery) and two questions. The experts were asked to analyze the literature and, based on the available validated data, to answer the questions if possible.
4.3 The committee committee
It was made up of :
- R. Legré: University Professor, Surgeon, Head of the Hand and Plastic Surgery Department, Hôpital de la Conception, Assistance Publi- que-Hôpitaux de Marseille, France;
- J.F. Schuhl: surgeon, national expert approved by the Court of Cassation, Rouen, France;
- F. Moutet: Surgeon, University Professor, Head of the Hand and Burn Surgery Department, Grenoble, France.
The experts were asked to give their answer at a round-table discussion held during the national congress of the Société française de chirurgie de la main (French Society of Hand Surgery). In the absence of certainty, the experts would pose questions to all the surgeons present, in search of a strong professional consensus.
Finally, a panel of judges attended the round-table and took notes, so as to produce a written summary on the same day and provide answers to the questions posed, if possible. An initial document drafted by one of the jury members was annotated and corrected by all jury members, resulting in the current document, validated by all jury members.
The jury was made up of :
- Dumontier (hand surgeon, Chairman of the Jury), F.-J. Pansier (magistrate at the Bobigny High Court), G. Chatellier (professor of epidemiology and medical informatics),
- Bernard (professor of infectious diseases), F. Chaise (hand surgeon, orthopedist), D. Maladry (hand surgeon, plastic surgeon).
To raise awareness of the problem of antibiotic prophylaxis among those of us who may not be familiar with it, an inau- gural lecture was given on the individual and collective risks of antibiotic use by Pr Drouin, anaesthetist, university professor, head of the Department of Anaesthesia and Intensive Care, Assistance publique des hôpi- taux de Marseille, Hôpital de la Timone, Marseille, an expert in these issues and having already taken part in two SFAR consensus conferences.
5. The experts : the questions asked à at room
(The answers are expressed at percentage from voters, the number from voters is registered à right from every table).
5.1 Should antibiotic prophylaxis be considered for
an isolated flexor lesion managed beyond the 24th hour?

5.2 Should antibiotic prophylaxis be considered for
a patient with a complex flexor lesion (e.g. total anterior wrist hemisection)?
5.3 Is it necessary consider a antibiotic prophylaxis in the plug at load surgical a fracture open osteosynthesized in visit six hours following the accident ?

5.4 Should antibiotic prophylaxis be considered in surgical procedures involving bone or osteoarticular
of the hand?

5.5 Should antibiotic prophylaxis be considered in
hand revision surgery, including bone or osteoarticular procedures, apart from postoperative infections?


5.6 Should antibiotic prophylaxis be considered in patients with no previous history of antibiotic treatment
of hand surgery other than bone or implant surgery?

5.7 Should antibiotic prophylaxis be considered in diabetic patients with
hand surgery other than bone or implant surgery?

5.8 Should antibiotic prophylaxis be considered in
first-line, implant-assisted hand surgery in patients with no previous history?
5.9 Should antibiotic prophylaxis be considered in
first-line, implant-assisted hand surgery in fragile patients?

5.10. Faut-il envisager une antibioprophylaxie lors
de gestes chirurgicaux de première intention sur des zones dites à risque (pli IPP, repli unguéal, plis palmaires…) chez des patients sans antécédents ?

5.11. Faut-il envisager une antibioprophylaxie lors
de gestes chirurgicaux de première intention sur des zones dites à risque (pli IPP, repli unguéal, plis palmaires…) chez des patients avec antécédents ?

6. The conclusions of the jury
Visit jury had à answer à several questions installed by the committee organization. For this, it a taken at account the notice from experts when exist from certainties scientists and the notice from the room à which several questions have summer installed à the research a consensus professional when no
scientific certainty. The jury noted that no Cochrane review was available on antibiotic prophylaxis in hand surgery.
The following recommendations made by the jury apply to all patients with the exception of :
- patients with valvulopathy. In these patients, a consensus conference of the Société des infectiologues de langue française recommends an- tibioprophylaxis, even though giving it does not seem to completely eliminate the risk of infection;
- insulin-dependent diabetic patients – for whom there is no certainty, but for whom it is customary to prescribe antibiotic prophylaxis. Patients with balanced, non-insulin-dependent diabetes do not warrant differentiation from the general population. These patients are at greater risk of infection, but the frequency of this risk does not appear to be reduced by antibiotic prophylaxis. This group cannot therefore be differentiated, but should be monitored more closely.
- immunocompromised patients (rheumatoid arthritis and all patients on corticosteroids, HIV-infected patients) should not be distinguished from the general population either. The risk of infection is greater in these patients, but the literature does not suggest that antibiotic prophylaxis reduces this risk. Given the low incidence of post-operative infections in hand surgery, this population need not be singled out.
6.1 What is the role of antibiotic prophylaxis in the management of simple hand wounds?
Simple wounds are defined as all lesions involving cutaneous penetration of the hand or fingers, but not accompanied by bone or joint lesions, or opening of the flexor sheath.
An analysis of the literature reported by the experts shows that there is no indication for antibiotic prophylaxis, whatever the delay before the procedure if it does not exceed 48 hours, and whatever the patient’s condition (diabetic, immunodeficient, etc.). There is no justification for discontinuing antibiotic therapy instituted prior to surgery (e.g., for infectious pulmonary or ENT diseases).
Analysis of the literature shows that this attitude is justified if accompanied by appropriate management: abundant wound cleansing, high-quality surgical trimming.
6.2. Place from antibiotic prophylaxis at from the plug at load from wounds complexes from the hand ?
A difference exists in the literature between visit wounds domestic and industrial and visit wounds original agricultural
whose wounds contain different types of germs. This difference is not justified by the literature in terms of the value of postoperative infection rates. There is no evidence in the literature to show the benefit of antibiotic therapy in decaying wounds, particularly those observed in agricultural accidents.
It has also been shown that antibiotics do not diffuse into necrotic tissue.
In these cases, the importance of appropriate management, including washing, brushing and mechanical removal of soiling, and high-quality surgical trimming, is underlined. Antibiotic prophylaxis does not appear to offer any advantage in the prevention of postoperative infections.
There is no evidence to suggest that a long delay before surgical management justifies a change in this attitude, but the literature is poor in this area and no validated recom- mandation can be offered.
Operating time is one of the most important factors in the risk of infection, and the clear limit is more than two hours of surgery. Although there are no arguments in the literature on the benefit of antibiotic prophylaxis in this type of complex lesion, an operating time of more than two hours may justify antibiotic prophylaxis, but the jury is unable to make any recommendation in the absence of available data.
6.3. Place of antibiotic prophylaxisat of the intake in care of fractures ?
The literature shows that there are no indications for antibiotic prophylaxis in closed hand fractures treated by osteosynthesis, in contradiction with the opinion of the hand surgeons present in the room.
In the case of open fractures, the risk of infection is not precisely known, but appears to be well below 1%. The potential benefit of antibiotic prophylaxis will therefore be largely outweighed by the individual (and collective) risks of that same antibiotic prophylaxis. There is therefore no indication for antibiotic prophylaxis in open fractures, even those treated by osteosynthesis, subject to soft tissue and medullary trimming. As hand surgery has evolved differently, extrapolation of studies on open diaphyseal leg fractures to diaphyseal hand fractures cannot reasonably be applied here.
Since the duration of the operation is one of the most important factors in the risk of postoperative infection, a procedure lasting more than two hours on a bone or osteoarticular segment may justify antibiotic prophylaxis. In practice, this is not the total duration of the operation, but the time spent on a segment (in hand surgery, an operation lasting more than 2 hours on a single finger may justify antibiotic prophylaxis). Thus, a re-implanta- tion digital which would last more from two hours would justify a antibiotic prophylaxis, even if the time bone is short. A reimplantation multi-digital relief also a pre– vention.
6.4. Place of antibiotic prophylaxis during during procedure controlled involving a procedure bone or osteoarticular ?
There is no evidence in the literature in favor of antibiotic prophylaxis. 64% of hand surgeons (128 votes) voted against the principle of antibiotic prophylaxis. Calculations of postoperative infection show that the risk is low, and that the potential benefit of such antibiotic prophylaxis would be largely outweighed by the individual risks of such prophylaxis (not to mention the collective risks).
There is no indication for antibiotic prophylaxis when performing osseous procedures (osteotomies and others) or osteoarticular procedures (arthrodeses and others) in controlled surgery.
6.5. Place of antibiotic prophylaxis during during procedure controlled of revision surgery involving a procedure bone ?
The literature provides no information on the preventive value of antibiotic prophylaxis. The opinion of the Société fran-çaise provides no additional information, since 56% of the 129 voters were in favor of antibiotic prophylaxis, which, given the numbers involved, corresponds to a shared opinion.
The SFAR consensus review considers that there is no need to modify any antibiotic prophylaxis initially given for late revision surgery (more than three weeks away).
If we reason “logically”, antibiotic prophylaxis is not indicated if the patient is not already “contaminated”, and conversely, if we fear previous contamination, it is more logical not to give antibiotics before taking intraoperative samples. It should also be borne in mind that systematic intraoperative sampling of patients undergoing surgery for the first time is of no use in predicting a possible postoperative infection. To be considered positive for antibiotic therapy, the same bacteria must be found in several samples (at least two). Antibiotic therapy may be requested after these samples, and modified or discontinued depending on the microbiological culture.
As the duration of the surgical procedure is one of the most important factors in the risk of postoperative infection, a procedure lasting more than two hours on a bone or osteoarticular segment may justify antibiotic prophylaxis. In practice, this is not the total duration of the procedure, but rather the time spent on a segment (in the practice of hand, a intervention from more from 2 hours on a only finger, can justify a antibiotic prophylaxis).
6.6. hand, a intervention from more from 2 hours on a only finger, can justify a antibiotic prophylaxis).
Analysis from the literature and the notice from experts allow from say that there a not indications à a antibiotic prophylaxis at surgery set from the hand do including not from gestures bone or joints.
6.7. Place of antibiotic prophylaxis during during surgery controlled with placement implants ?
No formal data exist in the literature. By extrapolation, antibiotic prophylaxis is considered indispensable in wrist prosthesis surgery (total radiocarpal prosthesis). Even if this attitude is scientifically debatable, given the small number of wrist prostheses fitted each year, antibiotic prophylaxis can be proposed without risk (individual or collective).
No reliable data are available for finger implants either. The rate of infection reported in the literature varies from 1 to 10. No recommendation can therefore be made. The meeting was generally in favor of such antibiotic prophylaxis. The jury’s opinion, although not a recommendation, is that antibiotic prophylaxis is probably not necessary, given the low risk of sepsis, the controlled nature of the surgery, the small size of the implants and the usually rapid nature of this type of surgery. Given the current state of knowledge, the surgeon cannot be blamed for the absence of antibiotic prophylaxis in a patient with a postoperative infection.
6.7. The choice of antibiotics
The germs encountered in hand surgery are, in the vast majority of cases, those encountered in orthopedic or plastic surgery. As the recommendations proposed in general reviews of the chi- rurgy literature {Hoffman, 1998 #20} are close to those of SFAR, the jury chose not to modify the SFAR recommendations. (http://www.sfar.org/antibiofr.html).
This attitude facilitates prescriptions for surgeons who do more than just hand surgery, limits the risk of prescribing errors, and limits the number of products available within an establishment for reasons of organization and cost.
The jury chose to recall the SFAR recommendations on the use of antibiotic prophylaxis. This must be
It is also important to note that the drug is “administered” (usually intravenously),
should always precede the operative procedure (within a maximum of 1 to 1.5 hours, and before tourniquet placement), if possible during induction of anesthesia, and last for a short time, usually during the operative period, sometimes 24 hours and exceptionally 48 hours. It should be shortened if studies allow. The presence of drainage from the surgical site does not allow these recommendations to be transgressed. There is no reason to prescribe reinjections when removing drains, probes or catheters”.
The antibiotics proposed are a first-generation cephalosporin (cefazolin, cefamandole, cefuroxime) and, in the case of allergy to betalactam antibiotics or suspected or proven colonization by methicillin-resistant staphylococcus, vancomycin. The jury also recalls that
“Selected protocols must be written, validated by the CLIN and the facility’s drug committee. These protocols must be affıked in the operating room”..

